Like New Again
Shoulder replacement options are transformational for arthritis patients and those with torn rotator cuffs
Many people know what it’s like to experience severe shoulder pain, which can result from osteoarthritis or from a torn rotator cuff, a network of tendons and muscles that stabilize the shoulder. While not as common as knee or hip replacements, many people have had shoulder replacement surgery, and it’s available right here in Central Texas at Baylor Scott & White in Marble Falls.
Orthopedic surgeon Adam Racusin, MD, is now performing less invasive, total and “reverse” shoulder replacement procedures, helping patients with severe osteoarthritis and rotator cuff injuries breathe a much-appreciated sigh of relief. Dr. Racusin comes to Baylor Scott &White following four years of active military duty that included time at Fort Hood and a one-year deployment in Afghanistan in 2011. After leaving the military in 2014, he completed a one-year fellowship in shoulder replacement surgery at San Diego Sports Medicine and Arthroscopy. “It’s a good procedure for people with end-stage arthritis of the shoulder, or irreparable rotator cuff injuries,” he says.
Total shoulder replacement
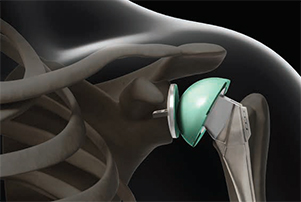
Patients with chronic shoulder pain from osteoarthritis are candidates for a total shoulder replacement, or total shoulder arthroplasty (TSA), an artificial replacement of the shoulder joint that uses a ball and stem to replace the damaged head (or ball) of the humerus, the long bone that runs from the shoulder to the elbow. When all conservative treatments, like physical therapy or steroid injections, fail to improve the symptoms, TSA becomes an option. “It’s debilitating for patients who don’t find symptom relief,” says Dr. Racusin, one of a few surgeons in the Marble Falls area who performs the procedure. “People lose strength and range of motion, and have difficulty doing very simple tasks, like reaching up to get something out of the cupboard, or washing their hair.”
 Dianne Jones, 76, was an ideal candidate for the TSA procedure. “I couldn’t blow dry my hair,” she says. “I couldn’t even pick up a pot filled with water. My family said I was driving with one arm. I believe that was true.” Before Mrs. Jones had the procedure, Dr. Racusin asked her, as with all his patients, to try other treatments before deciding to proceed with surgery. Mrs. Jones tried an injection without any improvement. “We always try to get people better without surgery – with steroid injections, physical or aquatic therapy, and other means – before going ahead with replacement,” Dr. Racusin says.
Dianne Jones, 76, was an ideal candidate for the TSA procedure. “I couldn’t blow dry my hair,” she says. “I couldn’t even pick up a pot filled with water. My family said I was driving with one arm. I believe that was true.” Before Mrs. Jones had the procedure, Dr. Racusin asked her, as with all his patients, to try other treatments before deciding to proceed with surgery. Mrs. Jones tried an injection without any improvement. “We always try to get people better without surgery – with steroid injections, physical or aquatic therapy, and other means – before going ahead with replacement,” Dr. Racusin says.
Recent advances in the size of the TSA implant are providing significant benefits to patients. Dr. Racusin uses what’s called a “stemless shoulder system”. He says, “Normally, you have to place a long stem into the humerus to get stability. The new component, which does not require instrumentation for the shaft, offers benefits that include less blood loss, and it’s easier to make adjustments.” This new device just received clearance from the Food and DrugAdministration for use in 2015, and is designed to minimize bone removal and soft-tissue disruption associated with the use of long-stem devices. The system reduces the procedure time, and especially meets the needs of younger patients who are reluctant to modify their lifestyles due to shoulder pain.
The rotator cuff
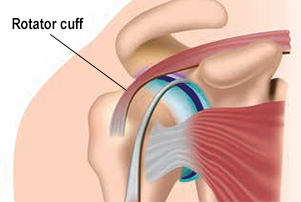 As people get older, many experience shoulder pain at night and find it difficult to get comfortable. This is often caused by an “impingement” or pinching of the rotator cuff, a network of tendons and muscles that connect the upper part of the humerus (arm bone) to the shoulder blade. The tendons of the rotator cuff provide stability for the shoulder and the muscles serve to strengthen movement, enabling the shoulder to rotate. Impingement can occur because the rotator cuff does not have much space to move, so it rubs against the undersurface of the bone – and over time, can be torn.
As people get older, many experience shoulder pain at night and find it difficult to get comfortable. This is often caused by an “impingement” or pinching of the rotator cuff, a network of tendons and muscles that connect the upper part of the humerus (arm bone) to the shoulder blade. The tendons of the rotator cuff provide stability for the shoulder and the muscles serve to strengthen movement, enabling the shoulder to rotate. Impingement can occur because the rotator cuff does not have much space to move, so it rubs against the undersurface of the bone – and over time, can be torn.
Rotator cuff injuries are common among athletes and older people, as well as individuals with jobs that require repetitive overhead motions. In 2008, almost two million people saw a physician about a rotator cuff issue. When a tear occurs, the simplest activities can become painful. Left untreated, the tear can get larger over time and shoulder replacement surgery can be an option.
Relief for torn rotator cuffs
A “reverse” shoulder replacement technique is available for people with completely torn rotator cuffs who are experiencing severe arm weakness, or those with severe arthritis and a torn rotator cuff who have had a previous failed procedure. Dr. Racusin says this procedure’s ideal candidate is age 70, and the youngest patient he’s performed the procedure on is age 61.“He does a lot of manual labor and he’s very happy with his results,” says Dr. Racusin.
The procedure is new in the past decade, and it’s quickly gaining popularity. Dr. Racusin explains that in the “reverse” shoulder replacement surgery, the socket and metal ball implants are switched: the ball attaches to the shoulder bone and the socket attaches to the upper arm bone so that patients can use their deltoid muscle (instead of the torn rotator cuff) to lift their arms.
Recovery time
Typically, patients who undergo shoulder replacement surgery are able to go home the day after the procedure. The recovery period includes approximately four to six weeks in a sling, accompanied by physical therapy. Generally, patients are able to return to daily activities within two to three months, and to more rigorous activities like golf or other sports in six months.
Mrs. Jones’s recovery took longer. “The surgery itself was a piece of cake; there was nothing to it,” she says. “Recovery was long, though, and I just had to be patient. I went to therapy three times a week, and did it every day at home for about five months. Now, I have full use of my arm.”
“For patients who go from having a shoulder that doesn’t move, and is chronically painful to having a shoulder that has functional use and does not hurt, the surgery is a godsend,” saysDr. Racusin. “Patients are so much better than they were, so they’re extremely satisfied.”
Read more in this issue